We most often associate cardiovascular diseases with blood pressure, cholesterol, and lifestyle. However, emotions such as chronic stress, tension, anxiety, and depression have an equal impact on them. They weaken motivation, worsen compliance with recommendations, accelerate inflammatory processes, and lead to metabolic disorders.
It is becoming increasingly clear that physical and mental health do not function separately. That is why care that combines these two perspectives is so important.
Primary care – the place where problems are first noticed
The most natural place to detect the first signs of a mental health crisis is in primary care. This is where patients visit regularly, and where their family doctor knows their history, life context, and how they have responded to stress in the past.
Prof. Donata Kurpas emphasizes: “In primary care, we look at the patient holistically – in their family, social, and professional context, with the full spectrum of stressors and health burdens.”
In practice, this means that the family doctor is the first to notice subtle changes: sleep disorders, chronic tension, decreased energy, social withdrawal, or a decline in previous activities. These changes can be an early sign of depression or anxiety disorders – problems that increase the risk of heart disease and hinder the treatment of existing diseases.
As Prof. Kurpas notes: “Early identification of these disorders allows for effective interventions to be implemented and breaks the growing feedback loop between psychological stress and somatic burden.”
Why is integrated care more effective?
Combining psychological support and cardiac education in a single setting provides patients with a sense of security, understanding, and control over their disease. This translates into:
- greater motivation for treatment,
- better adherence to pharmacotherapy,
- more effective lifestyle changes,
- fewer hospitalizations,
- and improved quality of life. and bonds
Prof. Kurpas points out: “Patients who receive both emotional support and education show better therapeutic adherence and a greater sense of security.”
This approach reflects a growing awareness that a patient is not a set of medical parameters, but a person with emotions, fears, and limitations.
New ESC guidelines – nurses as therapeutic partners
A new document from the European Society of Cardiology emphasizes the exceptionally important role of nurses in the care of patients with cardiovascular disease.
Prof. Izabella Uchmanowicz points to a fundamental change in approach: “This is a shift away from the ‘we treat the disease’ model towards ‘we support people living with chronic disease’.”
The most important elements identified in the guidelines are:
- Multidisciplinary team
Nurses are not merely executors of recommendations, but partners – they co-plan therapy, monitor symptoms, and coordinate the flow of information.
- Process-based education, not one-off
“One-off advice is not education – it must be process-based and repeatable,” notes Prof. Uchmanowicz. Education must be personalized, tailored to the patient’s age, experience, and life situation.
- Self-monitoring
Patients who recognize the first symptoms of deterioration (swelling, shortness of breath, weight change) are less likely to end up in the hospital. The nurse’s role is to teach them these skills.
4. Inclusion of psychological and social aspects
Depression, anxiety, and caregiver burden are an integral part of the clinical picture.
5. Telemedicine and modern communication
Apps, remote monitoring, and constant contact with a nurse improve continuity of care.
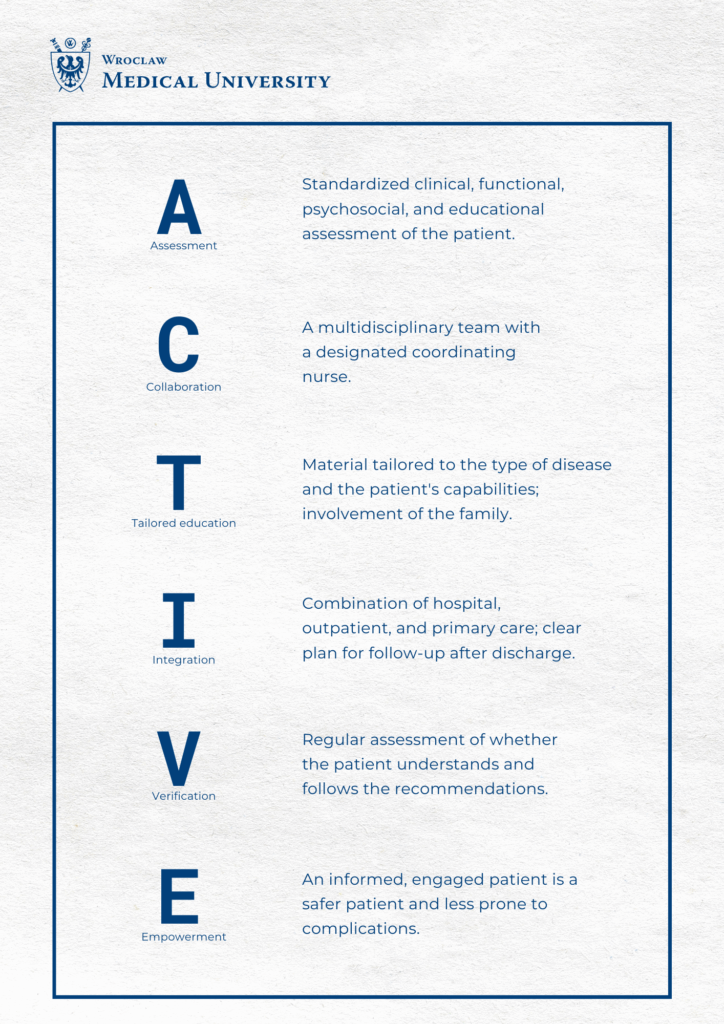
Polish centers are ready for this model
According to Prof. Uchmanowicz, many facilities in Poland already have the appropriate staff, tools, and technologies to fully implement ACTIVE principles. One example is the Institute of Cardiology at the University Clinical Hospital in Wrocław, where some of these activities have been in place for a long time.
Summary: a new standard of care for cardiology patients
Understanding that heart health and mental health form a single system changes the way we look at patients. The family doctor becomes the first line of early detection of mental disorders, and the nurse becomes a key partner in guiding the patient through the entire treatment process.
This approach—holistic, empathetic, and collaborative—is the future of modern cardiology and the foundation for a long, safe life for patients.
This material is based on the article:
2025 ESC Clinical Consensus Statement on mental health and cardiovascular disease: developed under the auspices of the ESC Clinical Practice Guidelines Committee: Developed by the task force on mental health and cardiovascular disease of the European Society of Cardiology (ESC)
Endorsed by the European Federation of Psychologists’ Associations AISBL (EFPA), the European Psychiatric Association (EPA), and the International Society of Behavioral Medicine (ISBM)
European Heart Journal, Volume 46, Issue 41, November 1, 2025, Pages 4156–4225,
Héctor Bueno, Christi Deaton, Marta Farrero, Faye Forsyth, Frieder Braunschweig, Sergio Buccheri, Simona Dragan, Sofie Gevaert, Claes Held, Donata Kurpas, Karl-Heinz Ladwig, Christos D Lionis, Angela H E M Maas, Caius Ovidiu Merșa, Richard Mindham, Susanne S Pedersen, Martina Rojnic Kuzman, Sebastian Szmit, Rod S Taylor, Izabella Uchmanowicz, Noa Vilchinsky, ESC Scientific Document Group