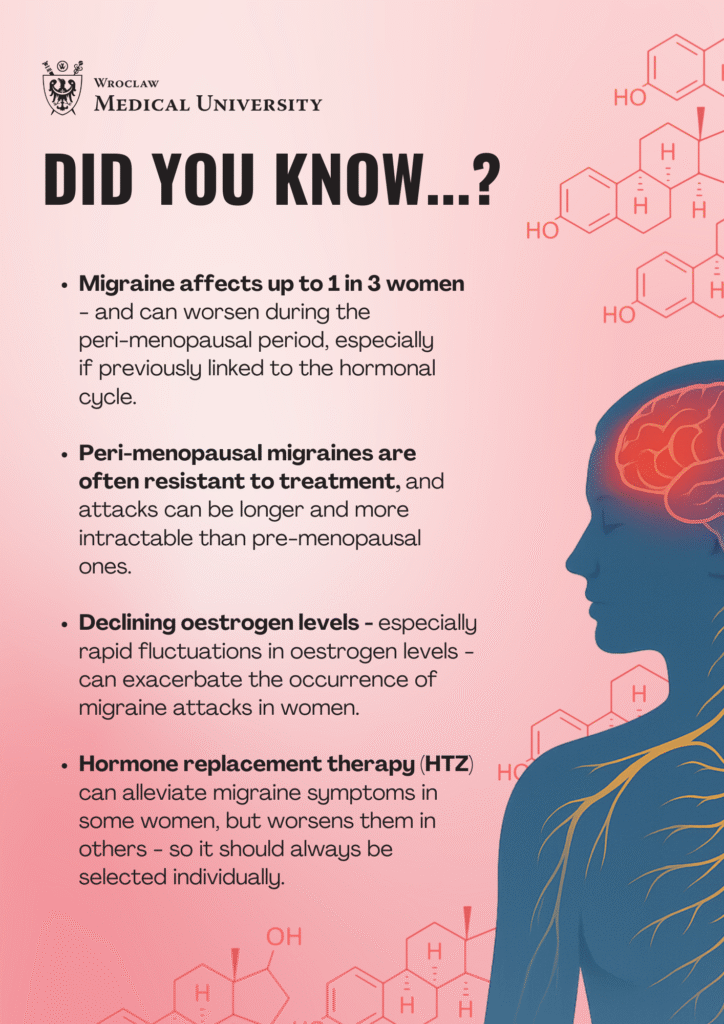
Fluctuations in estrogen levels during the perimenopausal period may exacerbate migraine, according to a review of research published in the journal Neurology and Therapy by Professor Marta Waliszewska-Prosół from the Department of Neurology at Wroclaw Medical University. The paper reveals the complex relationship between migraine and the hormonal balance of menopausal women.
Estrogen paradox
Migraine is one of the most common neurological diseases, affecting up to one billion people worldwide, the vast majority of whom are women. This gender imbalance has its origins in, among other things, the endocrine system. Estrogens – hormones crucial for reproductive health – also affect the vascular and nervous systems, playing an essential role in the pathophysiology of migraine.
During the perimenopausal period, when hormone levels fluctuate significantly, migraine often intensifies. So-called menstrual migraines become particularly acute, which, as the authors of the study point out, are more troublesome, longer, and less responsive to treatment than migraines independent of the hormonal cycle.
Perimenopause – a time of increased symptoms
Although migraine diminishes in some postmenopausal women, in many, the symptoms persist or even worsen. The perimenopause period, spanning several years before and one year after the last menstrual period, is associated with irregular and rapid decreases in estrogen, which may provoke more frequent headache attacks. The authors cite evidence suggesting a link between rapid hormonal changes and activation of neuroinflammatory and vascular systems.
As Prof Marta Waliszewska-Prosół points out: “Perimenopausal patients, in addition to the hormonal revolution significantly affecting the whole body, also experience work-life revolutions that affect both physical and mental health.” Work-related stress, new social roles, and comorbidities – can all further aggravate migraine complaints. “All this often covers up the problem of migraine, which, however, is naturally exacerbated under the influence of these factors.”
Therefore, as the researcher points out, a holistic approach is essential, including self-observation, psychological care, managing the course of migraine, and vigilance on the part of general practitioners (GPs). “Life hygiene is then paramount – the regularity that migraine most “likes.” Regular sleeping hours (not too long, not too short, no sleeping off weekends), meals, adequate hydration – with clean water (…). Finally, as in all diseases, physical activity is beneficial. I always recommend to my patients that they find a hobby and try to do something for themselves and only for themselves :).”
Therapy: hormonal or targeted?
The use of hormone replacement therapy (HTZ) in the treatment of migraine is controversial. In women with migraine without aura, it may bring improvement, but in patients with migraine with aura, HTZ may increase the risk of cardiovascular complications.
Therefore, there is a need to develop separate therapeutic guidelines for this patient group. “Currently, we, as the Polish Headache Society, would like to start working on the creation of good Polish recommendations that will also take into account this group of patients, which has always been somewhat overlooked,” announces Dr Waliszewska-Prosół. In her opinion, it is imperative to consider comorbidity, including cardiovascular risk.
In recent years, much hope has been raised by new therapies targeting the neurotransmitter CGRP (calcitonin gene-related peptide), which plays a key role in the pathomechanism of migraine. Monoclonal antibodies against CGRP represent a promising therapeutic alternative, especially for women in whom traditional treatments have failed.
Migraine and depression: a double burden
The review also highlighted the increased co-occurrence of migraine with mood disorders – especially depression and anxiety – during menopause. The authors point to a common neurobiological axis of migraine and depression related to, among other things, the serotonergic system. This highlights the need for a holistic approach – encompassing not only physical pain but also the psychological wellbeing of female patients.
The authors of this article Marta Waliszewska-Prosół, Giovanni Grandi, Raffaele Ornello, Bianca Raffaelli, Marcin Straburzyński, Claudio Tana, Paolo Martelletticall for greater awareness among physicians of the specificity of migraine in menopausal women. Treatment should be tailored individually, taking into account the patient’s neurological symptoms, hormonal status, comorbidities, and preferences. And above all – taking into account her lifestyle, mental and physical burdens, and needs, which change with age.
When you have a headache:
- Keep a migraine calendar. Record each day with a headache – its intensity, duration, and any triggers. This will help your doctor choose a more effective treatment.
- Take care of the regularity of your day Migraine’ likes’ routine. Try to: sleep regularly (not too short and not too long; 7-8 hours is the gold standard), eat at regular times, avoid dehydration – drink mainly pure water, not juices or herbs, which rehydrate less well.
- Avoid triggers. These may include: alcohol, certain foods, harsh light, noisy surroundings.
- Take care of your mental health. Patients in the perimenopausal period experience work-life revolutions in addition to the hormonal revolution. It is, therefore, worthwhile to: consult a psychologist or psychiatrist, identify and alleviate stressors, do not underestimate depressive or anxious states.
- Be physically active. Movement is not only supportive of general health – it can also reduce the frequency of migraine attacks. Find an activity you enjoy: walking, yoga, swimming, or dancing.
- Find something just for yourself. Time just for yourself relieves tension and supports mental well-being.
- Decide on hormone therapy with caution. HTZ can bring relief, but in women with migraine with aura, it also carries a risk of vascular complications. The decision should be made on an individual basis, taking into account the type of migraine, age, other medical conditions, and lifestyle.
- Consult a neurologist. If your migraines worsen or you reach for painkillers more often, consult your doctor. It may be possible to include modern therapies (e.g., anti-CGRP antibodies) or adjust hormone replacement therapy if there are no contraindications.
This material is based on an article:
Menopause, Perimenopause, and Migraine: Understanding the Intersections and Implications for Treatment
Authors: Marta Waliszewska-Prosół, Giovanni Grandi, Raffaele Ornello, Bianca Raffaelli, Marcin Straburzyński, Claudio Tana & Paolo Martelletti
Doi: https://link.springer.com/article/10.1007/s40120-025-00720-2