The public debate on cannabis is dominated by a tone of normalization – less stigmatization, more freedom of choice. The promise of a ‘natural’ alternative to medicines. Meanwhile, science, although still incomplete, is painting an increasingly coherent picture of how phytocannabinoids affect reproduction and child development. A team of researchers from Wroclaw Medical University collected 64 papers on THC and CBD and pointed out that the endocannabinoid system, which marijuana ‘boosts’, is not a side corridor of physiology, but the very center of fertility control.
THC disrupts fertility
The CB1 and CB2 receptors affected by THC are located where the most critical decisions are made – in the hypothalamus and pituitary gland, in the ovaries and testicles, and in the placenta. The effect in men is a decrease in sperm concentration and total sperm count, poorer motility, and possibly lower testosterone levels. Studies also show epigenetic changes in sperm. After taking THC, small ‘markers’ remain on the DNA, which can affect the development of offspring.
In women, the picture is equally disturbing, with disorders of follicular maturation, ovulation, and endometrial receptivity. The studies analyzed described a shortened luteal phase and weaker embryo implantation. And this is only the beginning, because during pregnancy, THC does not stop at the placental barrier. It penetrates it, affecting angiogenesis and oxygen delivery to the fetus. It has been linked to placental failure, low birth weight (SGA), prematurity, and, as a consequence, more frequent hospitalization of newborns in intensive care. On top of that, THC is also present in breast milk. In regular users, its concentration can be many times higher than in the blood.
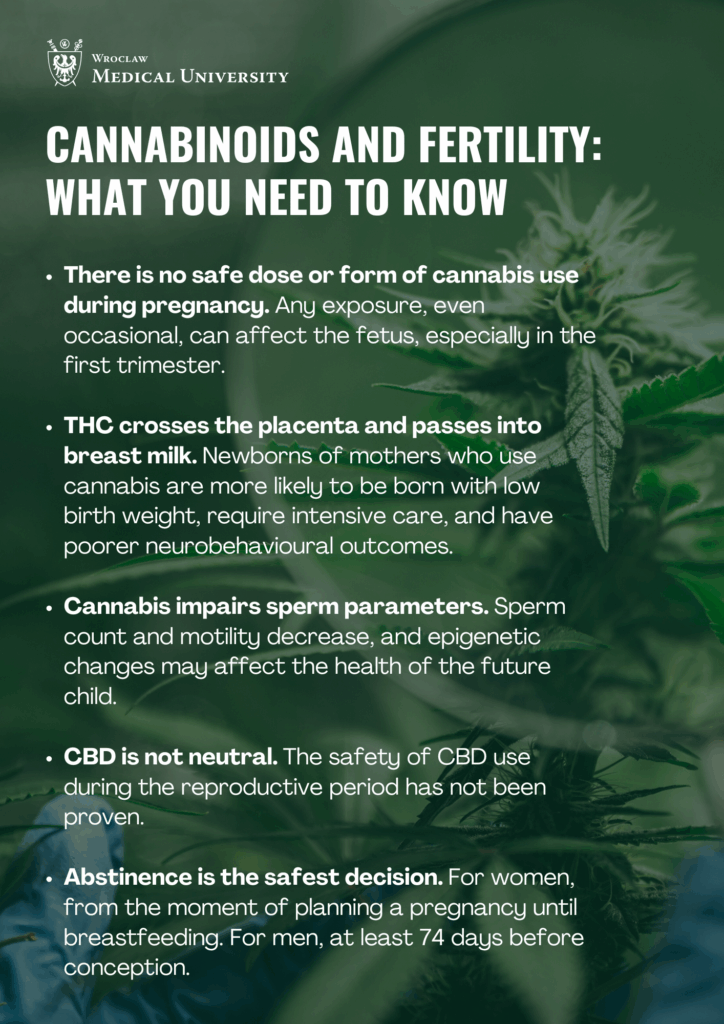
There is no ‘safe dose’
Currently, it is not possible to indicate a single, precise dose of cannabis that would be safe for fetal development or fertility, emphasizes Michał Wesołowski, MD, from the Department of Physiology and Pathophysiology at the Medical University of Wrocław, the lead author of the publication. ‘The more frequent and regular the use, especially of products with high THC concentrations, the greater the likelihood of adverse effects. The critical period is the first trimester of pregnancy, when the foetus’s organs and nervous system are developing,’ he points out.
The researcher notes that, although there is no clear safety threshold, biology is relentless. “From a public health perspective, it is recommended that women planning to become pregnant, who are pregnant or breastfeeding should completely stop using cannabis. Men planning to have children are also advised to abstain for at least 74 days, i.e. for the duration of spermatogenesis.
Pregnancy and THC
What about children exposed prenatally? Studies primarily focus on tracking cognitive functions and behaviors, including attention and memory deficits, impulsivity, and academic difficulties. Some data also point to metabolic ‘programming,’ i.e., a greater tendency towards obesity and higher blood sugar levels in childhood. Behind the mechanism that triggers this cascade is a mixture of dysregulated CB1 signaling, cellular stress, and epigenetic modifications.
There is no safe form of cannabis
Although different forms of cannabis consumption have different exposure profiles, none of them are risk-free, explains Dr Wesołowski. Smoking cannabis involves smoke toxins, vaporization, and concentrates deliver higher doses of THC, and edibles encourage uncontrolled consumption of larger amounts. Even CBD does not have a documented safety profile.
The review highlights the limitations. Exposure measurement can be inaccurate. It is based on declarations rather than biomarkers. But also, the cannabis of 2025 is not the same plant as it was two decades ago. It is now available in new, stronger concentrations, as concentrates, edibles, and vapes.
Added to this is the co-use of alcohol and nicotine. But even after all the hype is stripped away, the message remains clear: fertility and foetal development are sensitive to cannabinoids.
This is not a moral crusade. It is a call for proportion. In a world that is rightly moving away from punishing possession, we should be equally consistent in investing in education. Doctors need simple screening tools and clear guidelines. Patients need alternatives with proven safety (e.g. for nausea during pregnancy). Men planning fatherhood need information that ‘recreation’ can affect sperm parameters, and not just on weekends.
Legalization changes the law. Biology remains the same. When planning a pregnancy, during pregnancy and while breastfeeding, it is better not to take any risks. Freedom of choice is not about ignoring the costs, but about making decisions with full awareness of their price. In the case of cannabis, that price may be higher than we would like to believe.
This material is based on the article:
Effects of Phytocannabinoids on Reproductive System and Prenatal Development: Mechanisms and Clinical Implications
Authors: Michał Wesołowski, Aleksandra Sobaś, Kamil Biedka, Jakub Karwacki, Jakub Bulski, Katarzyna Błaszczyk, Kacper Żełabowski, Oliwia Ziobro, Filip Jacek Maj, Karol Sornat, Agata Estreicher, Anna Klasa, Andrzej Dłubak, Tadeusz Sebzda
J. Clin. Med. 2025, 14(18), 6494; https://doi.org/10.3390/jcm14186494